Diagnosing and
Treating Your
AR Patients
Be the determining factor that gives your patients access to timely treatment.*

The prevalence of AR
The prevalence of AR has been difficult to determine due to the many factors that go into the diagnosis. Even patients with chronic severe AR can spend years with normal left ventricle (LV) function and exhibit no symptoms. According to the Framingham Heart Study1 :
TABLE 1. Prevalence of AR in the Framingham Offspring Study:
| 50-59 | Age 60-69 |
70-83 | |
|---|---|---|---|
| Men | (n=433) | (n=359) | (n=91) |
| None | 91.1% | 74.3% | 75.6% |
| Trace | 4.7% | 13.0% | 10.0% |
| Mild | 3.7% | 12.1% | 12.2% |
| ≥Moderate | 0.5% | 0.6% | 2.2% |
| Women | (n=515) | (n=390) | (n=90) |
| None | 92.4% | 86.9% | 73.0% |
| Trace | 5.5% | 6.3% | 10.1% |
| Mild | 1.9% | 6.0% | 14.6% |
| ≥Moderate | 0.2% | 0.8% | 2.3% |
AR is undertreated
Even symptomatic patients that have been diagnosed with severe aortic regurgitation often do not receive necessary treatment.
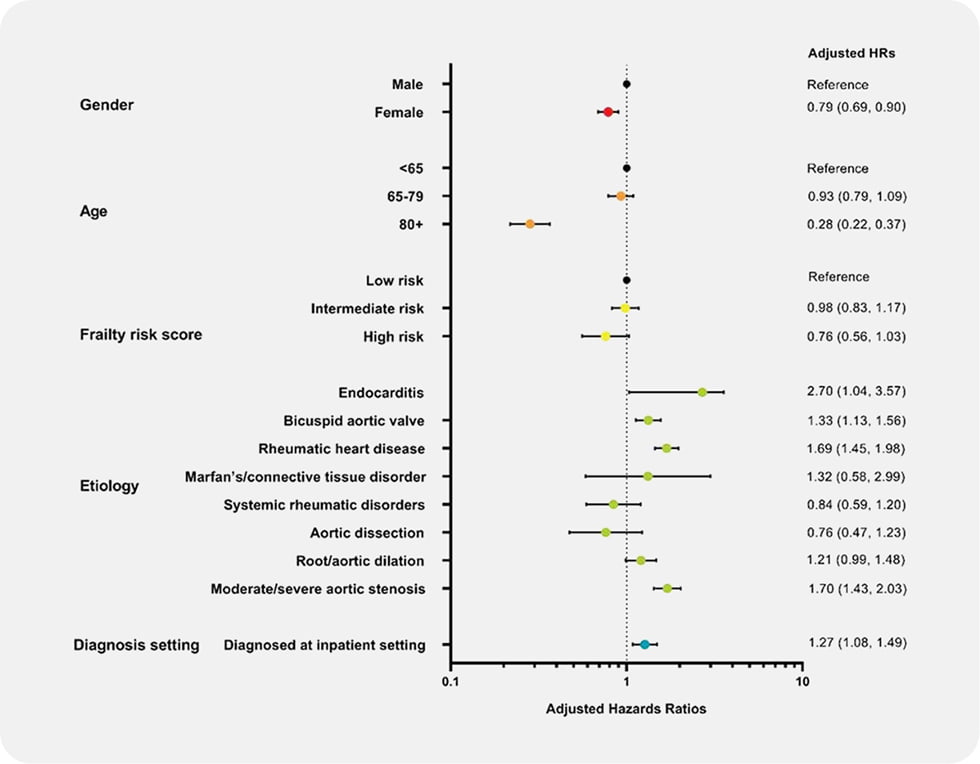
From a final cohort of 4,608 symptomatic severe AR (ssAR) patients2 :
- Only 25.7% of patients underwent SAVR within 1 year of diagnosis
- Factors that negatively impacted the likelihood of SAVR treatment include
- Female gender
- Age (80+)
- Low LVEF (<35%)
Left untreated, severe aortic regurgitation will lead to LV dilation, decompensation of the left ventricle, and heart failure.
The pathophysiology of chronic, severe AR
Asymptomatic patients with LV systolic dysfunction will rapidly progress to symptoms (>25% per year).3
Once patients become symptomatic, their mortality rate is greater than 10% per year.3
The progression of AR4:






Without treatment, AR is life-threatening
Once AR has progressed to the symptomatic stage, it becomes a life-threatening disease.
A study of patients with severe aortic regurgitation found the patient’s NYHA class and the presence of symptoms to be predictors of survival. Survival rates were significantly lower in symptomatic patients than in asymptomatic patients, and NYHA class I and II patients had significantly different survival rates than patients in class III and IV at baseline.5
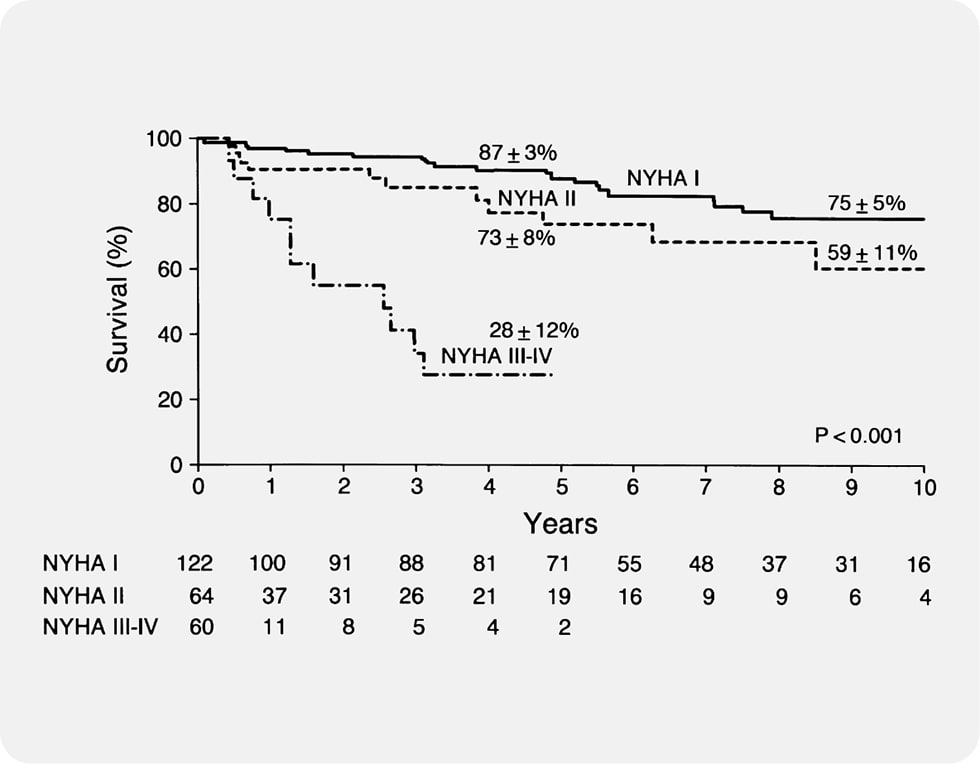
If the patient is symptomatic, mortality increases to 9.4% per year.5
If the patient is NYHA Class III/IV, mortality further increases to 24.6% a year.5
In another study, from a final cohort of 4,608 ssAR patients, mortality was 9% for patients who received SAVR within 1 year of diagnosis. In comparison, mortality was 24% in patients who did not receive treatment.2
Early AR diagnosis is the key to timely treatment
Echocardiography is the most important tool to diagnose AR, grade its severity, and determine the follow-up frequency.6
Asymptomatic severe AR patients should receive echocardiography every 6-12 months.
Symptomatic patients should immediately be considered for intervention.7
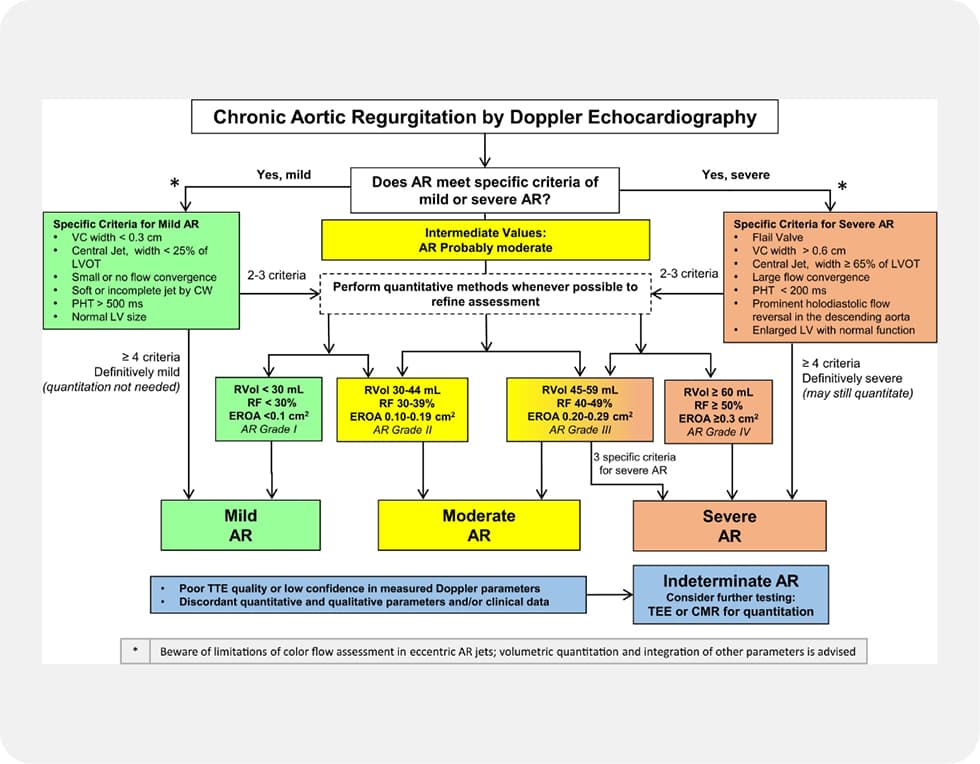
But while echocardiography is a crucial tool in assessing patients with aortic regurgitation, it is not the only tool. Fully evaluating AR should be an integrative process that can include multiple parameters from different imaging modalities, including cardiac magnetic resonance (CMR) and cardiac computed tomography (CCT).

Once a patient has been diagnosed with AR, it is critical to refer them for treatment which will depend on the severity of the patient’s condition.
Treating severe AR
Fully treating and managing AR means preserving left ventricular function and providing optimal long-term outcomes for mortality and morbidity.6
The most effective treatment method will depend on the severity of the patient’s condition and the patient’s overall health.

Medical management
Medical management can alleviate symptoms of AR in patients with high surgical risk, but it cannot treat the condition at its root and will not reduce or delay the need for AVR.
- There is no evidence that vasodilating drugs reduce the severity of AR or alter progression in patients with significant, chronic AR.6
- In a randomized trial, vasodilator therapy did not reduce or delay the need for AVR in patients with asymptomatic severe AR and normal left ventricular systolic function.8
- Vasodilator therapy also did not reduce regurgitant volume or left ventricular size and did not improve left ventricular function.8
- Despite medical management, patients still experienced higher-than-expected mortality at 10 years.5
- Despite medical management, the majority of patients required AVR, and 83% experienced a cardiovascular event.5
Once an AR patient is symptomatic, medical management is not sufficient.
SAVR

Surgical intervention is the most effective treatment and the recommended treatment method for patients with severe AR.
In a study of 1,417 patients with severe AR and preserved LVEF (>50%), patients who received AVR showed 13% mortality at 10 years as opposed to 29% mortality at 10 years for patients who did not receive AVR.9
However, only 25.7% of symptomatic severe AR patients receive SAVR within 1 year of diagnosis.2
Patients at an advanced age or with multiple comorbidities often are not able to undergo surgery, leaving them with few options.
TAVR†

Transcatheter aortic valve replacement is an alternative to surgery in patients with aortic valve disease and is often offered to vulnerable patient populations with higher surgical risks.
However, current TAVR devices are designed to treat aortic stenosis and are not approved for treatment of aortic regurgitation. When these TAVR devices are used off-label there are increased procedural risks and they have limited effectiveness in eliminating the AR.
Current TAVR devices designed to treat AS:
- Rely on calcification of the native cusps for anchoring10
- Involve a high risk of valve embolization or need for a second valve11
- Can potentially increase the risk for annular rupture and/or paravalvular AR10
The outcomes of using AS-specific TAVR devices to treat AR have not been favorable. A study evaluated TAVR procedures from January 2014 to September 2015 for severe AR with a commercially available self-expanding valve system. The mortality rate at 1 year was 25% for AR patients compared with 18.3% for AS patients.12
There is a clear need for a transcatheter device that is specifically designed to treat patients with severe aortic regurgitation. Clinical trials for these dedicated devices are currently underway in the US.
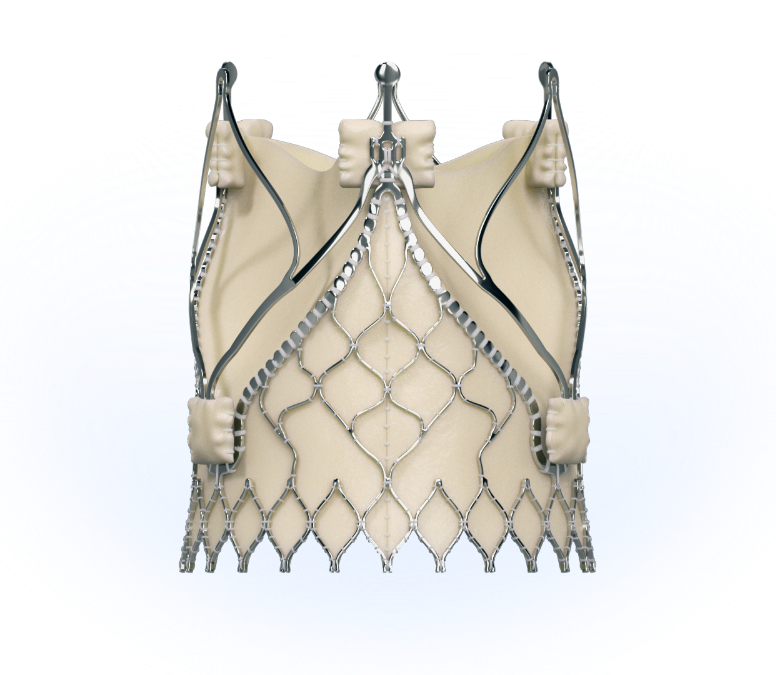
Introducing the Trilogy System
The JenaValve Trilogy System is the only TAVR device approved to treat patients with severe AR.
Contact Us
Looking to discuss treatment
options for your severe AR patients?
Contact us today.
1 Singh et al. Am J Cardiol 1999;83:897–902
2 Thourani et al. Structural Heart 2021; DOI:10.1080/24748706.2021.1988779
3 Bonow RO, et al. Circulation. 1998;98(18):1949-1984
4Bekeredjian R, et al. Circulation 2005;112:125-134
5 Dujardin K et al. Circulation. 1999;99:1851-1857
6 Maurer G. Heart 2006;92:994-1000
7 Otto CM, et al. Circulation. 2021;143:e72-e227
8 Evangelista A, et al. N Engl J Med 2005;353:1342-9
9 Mentias A, et al. JACC 2016;68(20):2144-2153
10Franzone A, et al. JACC Cardiovasc Interv 2016 Nov 28;9(22):2308-2317. DOI: 10.1016/j.jcin.2016.08.049
11 Testa L, et al. EuroIntervention 2014;10:739-745;
12 Anwaruddin, S. “Self-Expanding TAVR for Treatment of Aortic insufficiency: The STS/ACC TVT Registry Experience” Presented at: TCT 2018; September 22, 2018; San Diego, CA.
*To the extent this site contains information, reference guides and databases intended for use by licensed medical professionals, such materials are not intended to offer professional medical advice.
†US: CAUTION – Investigational Device. Limited by Federal (or United States) law to investigational use.




