About AR
Learn all about AR and its causes, symptoms, and possible treatment options.

What is AR?
Aortic regurgitation (AR) is a condition in the heart’s aortic valve, which impacts how blood flows through your heart.
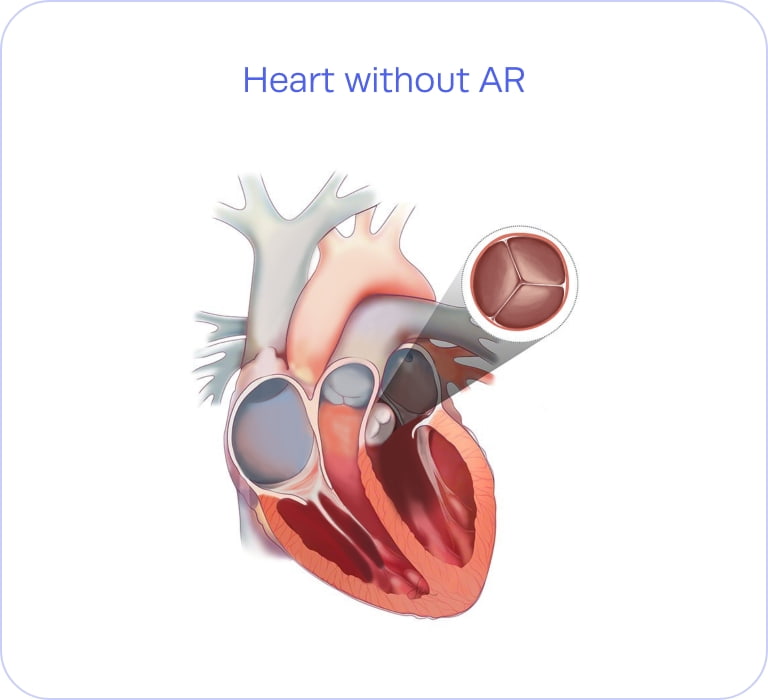
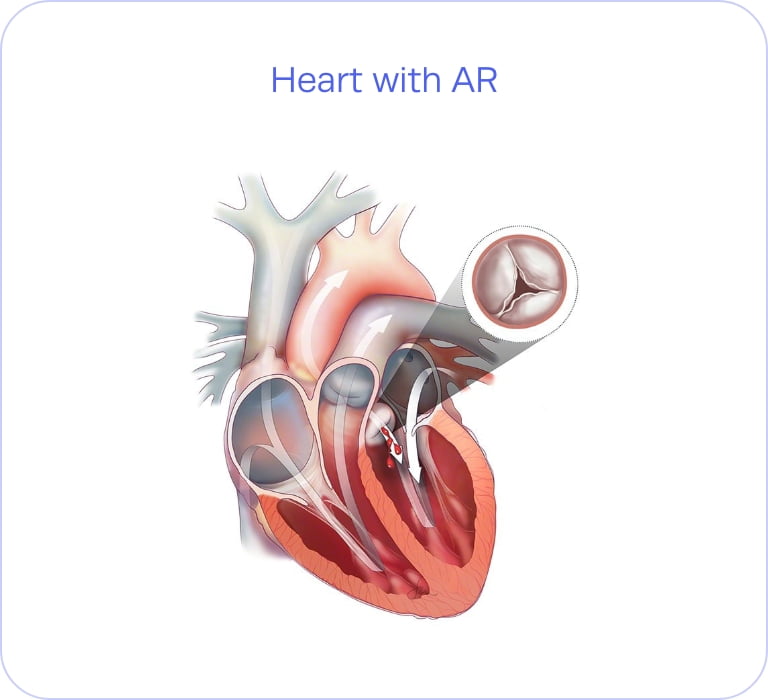
The aortic valve has three flaps (also known as leaflets) that open and close to pump blood into the heart. If the aortic valve doesn’t close or can’t close tightly enough, the blood can leak and flow backward into the left ventricle.
This leakage is what we refer to as aortic regurgitation—and if left untreated, it can lead to even more issues for your heart’s function and may even be life-threatening.
What can cause chronic AR?
Any condition or injury that damages your aortic valve could potentially cause AR. The most common causes of chronic AR in North America and Western Europe are congenital disease and degenerative disease1, including:
Congenital heart valve disease
If abnormalities in the aortic valve (such as bicuspid aortic valve) aren’t monitored by a doctor, they can lead to AR later in life.
Infection of the heart’s tissue (endocarditis)
This bacterial infection is one of the most common causes of chronic AR.
Rheumatic fever
If strep throat is not properly treated, it can damage the aortic valve and potentially cause severe AR.
Valve degeneration
The aortic valve tissue can weaken over time, which can lead to aortic regurgitation at a later age.
Aortic root dilation
The first part of the aorta exiting the heart (the aortic root) can become enlarged with age. This can cause separation in the leaflets and is one of the most common definable causes of severe AR.
Other connective and autoimmune diseases
Conditions like Marfan syndrome and lupus can potentially lead to AR.
Chronic AR is a progressive disease that worsens over time. Patients can live with mild aortic regurgitation for years, oftentimes without many symptoms. However, once symptoms appear, it is important to seek treatment before irreversible heart damage occurs.
FDA-approved clinical study
We’re now enrolling patients with AR to participate in the ARTIST Trial.
If you have been diagnosed with AR or are experiencing symptoms, you may be eligible for this trial.
Learn more
What are the signs and symptoms of AR?
Your doctor may diagnose you with aortic regurgitation even if you are not experiencing symptoms, as symptoms typically only appear once your condition has progressed to the later stages. Some of the most common symptoms include:
-
 Chest pain, discomfort, or tightness
Chest pain, discomfort, or tightness -
 Fatigue or weakness
Fatigue or weakness -
 Shortness of breath
Shortness of breath -
 Swelling in the ankles/feet
Swelling in the ankles/feet -
 Rapid, fluttering heartbeat (palpitations)
Rapid, fluttering heartbeat (palpitations) -
 Irregular pulse (arrhythmia)
Irregular pulse (arrhythmia) -
 Heart murmur
Heart murmur -
 Lightheadedness or fainting
Lightheadedness or fainting
These symptoms can appear on their own, or they can increase if you’re exercising or engaging in physical activity.
If you’re experiencing any of these symptoms, it’s crucial to speak with your doctor to discuss treatment options.
The prevalence of AR
Heart valve disease is progressive and becomes more common as people age. So as people live longer, heart valve disease becomes a bigger concern. Even though it’s more common than many realize, it often goes undiagnosed or untreated and many people may suffer from heart valve disease without knowing it. From a recent U.S. study2:
If you’ve been told you have AR, see if you qualify to join the ARTIST Trial.
Is AR undertreated in the US?

Severe AR has been undertreated in the US—most people in the US with severe AR don’t receive any treatment, even if they have options available to them. Studies have shown that there are gaps in the treatment of women, older individuals, and people with other heart conditions.3
The factor that has the most influence on whether you receive treatment is your primary cardiologist’s diagnosis and referral.3
Understanding your risk factors will help you to recognize when you should speak with your doctor about AR. You should contact your doctor if you have any of the following risk factors:
- Older age (70+)
- Certain heart conditions present at birth (congenital heart disease)
- History of infections affecting the heart
- Other heart valve conditions (such as aortic stenosis)
- High blood pressure
How is AR diagnosed?
Your doctor’s first test will be listening to your heart with a stethoscope. If they hear a whooshing sound between beats, that is a sign of abnormal blood flow through the valve, which could point to AR.
If your doctor believes you could have AR, they can use any of the following tests to check your heart more thoroughly and confirm your diagnosis:
Echocardiogram
This test uses sound waves to produce images of your beat, which can detect AR and determine its severity.
Electrocardiogram
This test uses sound waves to produce images of your heart, which can detect AR and determine its severity.
Chest X-ray
An X-ray can detect if your heart or aorta is enlarged, which could be a sign of AR. It can also check whether your lungs have been impacted.
Cardiac MRI
This test can be helpful when the echocardiogram images are not optimal. Cardiac MRI (also known as CMR) can provide accurate and reproducible measures of how much regurgitation is occurring in the heart.
Cardiac catheterization
In this test, your doctor will insert a catheter through an artery and into your heart to get a closer, more detailed look at your heart’s valves and chambers.
Exercise or stress tests
An exercise test can determine whether you have any signs or symptoms of AR and assess how far your condition has progressed.
How can AR be
treated?
Learn more about how your doctor can help you today.

1Maurer G. Heart 2006;92:994-1000
2https://www.census.gov/quickfacts/fact/table/US/AGE775223#AGE775223
3Thourani VH, et al. Structural Heart. 2021;5(6):608-618. DOI:10.1080/24748706.2021.1988779



